January 17, 2022 | Septal Perforations.
4 minute read
A septal perforation is a hole in the nasal septum, the structure that divides your nasal cavity into two halves. While there are many potential causes for a septal perforation, previous septal surgery is the most common reason for a perforation. Not everyone with a septal perforation may benefit from surgery, because many small perforations are often asymptomatic. However, larger septal perforations have been linked with nasal crusting, bleeding, pain, whistling, nasal obstruction and, when large enough, septal perforations can affect the appearance of the nose.
The septal perforation is a challenging defect to repair. Unfortunately, we cannot just insert a graft to close hole because the perforation also involves the membranes (mucosa) that cover the left and right sides of the septal as well. Therefore, when we repair the perforation, we aim to create a three-layered repair: one membrane closure on either side with a connective tissue graft in between. Other techniques of repairing septal perforations may use tissue from the forehead, mouth, or free grafts. The problem with these techniques is that the transferred tissues do not form the same tissue that lines the inside of the nose, so they will not make the normal mucus that the nasal tissue will, and the nose can still be dry and crust after surgery.
First, to repair the septal perforation, we must lift up the nasal skin and carefully expose the septal perforation. This can be difficult, especially if you’ve had septal surgery before and have scar tissue or if septal cartilage or bone had been previously removed and all that is left around the periphery of the perforation are the membranes that are stuck together. The dissection alone, just to expose the perforation can take over an hour.
Once the components of the perforation have been separated, we must close the defects. In our experience, the best results are achieved when nasal tissue is recruited to close the hole. We achieve this by recruiting your own nasal membranes from above and below the holes. This helps restore natural physiology to the nose. We do this on both sides, which is more effective at closing the perforation than repairing just one side alone. To further reinforce the perforation repair, a graft is placed between the repaired membranes, usually from a donor or taken from another anatomic location (e.g., scalp). Everything is then sutured together and protected with bilateral 0.5mm-thick soft silicone sheeting for two weeks. Because of the protective silicone sheeting placed after surgery and the swelling from the flaps used in the nose, you can expect nasal obstruction for at least one month after surgery.
Often, a septal perforation repair can take three hours. However, in many cases additional nasal surgery may be required. We find that in some cases where a septoplasty was done previously the septum may still be crooked so we must not only go through scar tissue to repair the perforation, but we must also revise the septoplasty to improve the airway. Sometimes, when the septal perforation is large enough there is also problem with a loss of support, because the anterior portion of the septum provides structural support to the nose. This may be seen as sagging or drooping of the nose and can compromise breathing. In such cases, cartilage grafts may be required to re-establish support for the nose to improve breathing. In such cases, rib cartilage harvested from the patient or from a donor may be needed to create these grafts.
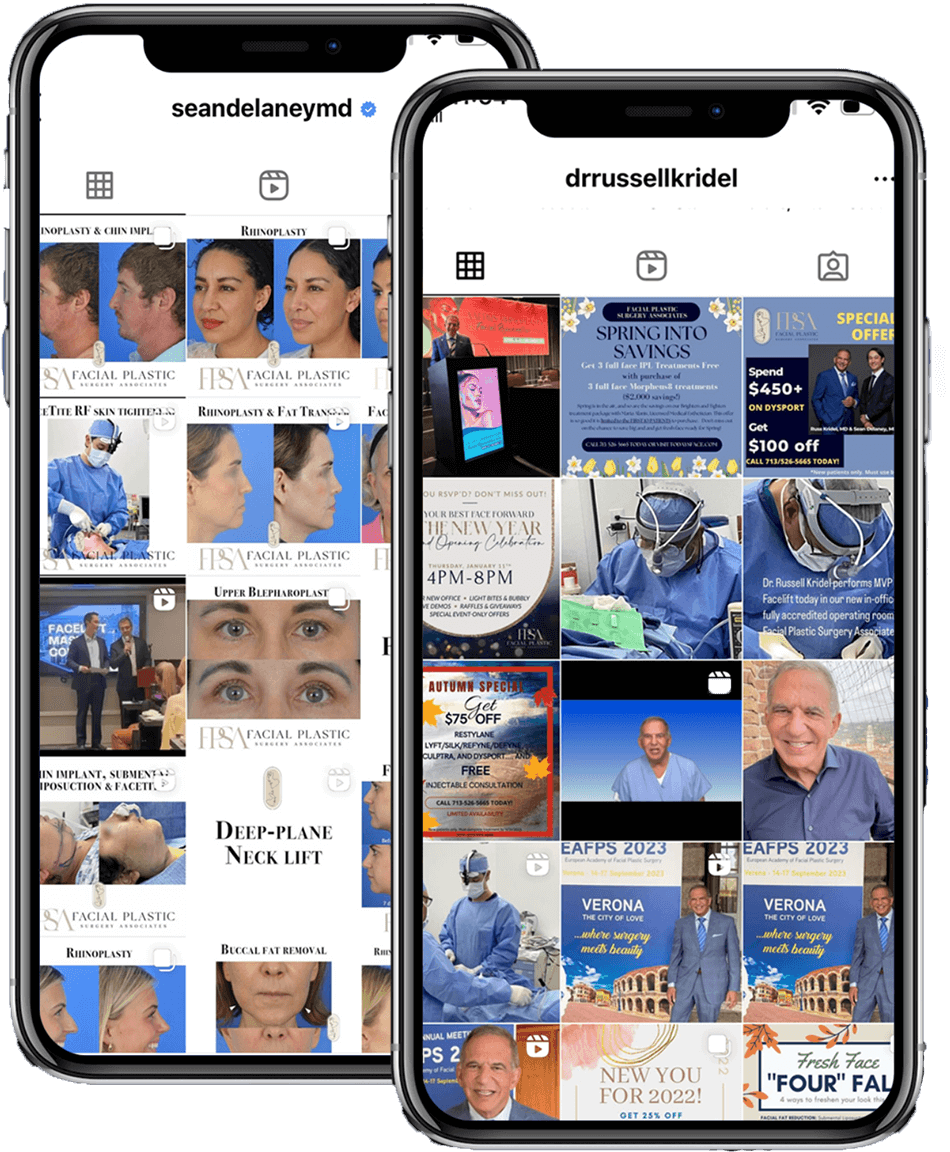
In summary, septal perforation repair is a complex operation that requires time and skill. The goal of the surgery is to use nasal tissue to restore normal nasal physiology. Septoplasty and Rhinoplasty can be safely performed in the same operative setting. In fact, Dr. Delaney and Dr. Kridel had published a peer-reviewed journal article in 2018 studying patients who underwent combined septal perforation repair and rhinoplasty and found that septal perforation closure success and rhinoplasty satisfaction were high and did not drop even when the two surgeries were performed in the same setting. Given the extended recovery period associated with the surgery, I recommend only the most motivated patients consider this operation.